By Sarah Anderson, PhD
When Carolina Tropini, Assistant Professor of Microbiology and Immunology, and Annie Ciernia, Assistant Professor of Biochemistry and Molecular Biology, teamed up for a mouse study of the effects of gut inflammation on the brain, they thought they might have mixed up the sex of the animals. To their fascination (and relief), the male reproductive organs had in fact failed to mature. “There was such a strong signal with the endocrine system. We never set out to discover that specifically, but the data just screamed at us that there was something important happening,” Tropini said.
The gut microbiome, the community of microbes inhabiting the gastrointestinal tract, continues to surprise scientists with the powerful and unexpected ways in which it interconnects with the rest of the body. “We're now understanding that the microbiota can affect any one of our organs,” Tropini said. Just as ibuprofen taken by mouth can alleviate a headache, gut microbes secrete signalling metabolites that are absorbed into the bloodstream and circulated systemically. Communication flows in both directions, as the microbes also respond to and modify biological molecules that penetrate the gut.
Following where the data led, Tropini’s and Ciernia’s research groups took on the task of untangling this intricate web of interactions along both the endocrine and neurological axes. In a recent study published in Brain, Behavior, and Immunity, the team reports how gut microbiome disruption influences behaviour, sex hormones, and brain structures in a mouse model of pediatric inflammatory bowel disease (IBD). “About a quarter of people with IBD have onset in childhood or adolescence, and they are very much understudied in terms of what the effects of early life inflammation might be on their developing brains and bodies and how that might have long-term impacts throughout the rest of their lives,” Ciernia said.

Carolina Tropini (left) and Annie Ciernia (right).
To simulate the intestinal injury characteristic of IBD, the researchers treated juvenile mice with dextran sodium sulfate, a chemical that damages the gut epithelial lining and induces inflammation. Genetic sequencing of stool samples revealed that the mice exhibited altered composition and loss of diversity in their gut microbiome species.
To examine the high-level effects of this gut microbiome disruption, the team tested the mice for behaviours related to memory, anxiety, depression, socialization, and mating. While the majority of behaviours were unperturbed, they found that the males lost their preference for the odor of female urine, a key aspect of mate seeking in rodents. With this piece of the puzzle in place (and the confusion about the shrunken reproductive organs in the male IBD mice cleared up), the researchers turned their attention to sex hormones.
In analyzing how the gut microbiome changed upon early life inflammation, the team observed a loss of microbes that express β-glucuronidases and β-glucosidases, enzymes that convert androgen hormones to their active form. The male IBD mice therefore displayed decreased activity of these enzymes and lower amounts of active testosterone, which likely underlies their impaired sexual development and behaviour.
Many of the missing microbes also produce short-chain fatty acids, anti-inflammatory compounds that help to maintain intestinal health and communicate with a range of bodily systems. Short-chain fatty acids can cross the blood-brain barrier and interact with brain cells such as microglia, immune cells that serve as the brain’s first responders to infection and damage. The researchers observed that the IBD mice displayed sex-specific deformities in microglial shape, potentially due to reduced levels of important short-chain fatty acid signalling metabolites. Further experiments are needed to understand how this change in brain morphology contributes to behavioural effects.
The researchers then sent their mouse brains to J.P. Yu, a professor of neuroradiology at the University of Wisconsin. He analyzed the samples using a non-invasive brain imaging technique that tracks the diffusion of water molecules as a measure of the density and orientation of brain cells in the tissue. The team found that brain regions with unusual microglial shape produced a distinct diffusion signature, suggesting that this tool could provide a biomarker of therapeutic response in clinical studies. “If we think that microglia are contributing to some kind of abnormal brain state, you could potentially treat patients with something that might be able to reverse that and actually have an in vivo measure of how effective the treatment was,” Ciernia said.
When it comes to developing new treatments for IBD, the malleable microbiome represents an attractive avenue to restore a healthy biological baseline. “We have coevolved with these bacteria for millions — if not hundreds of millions — of years. The advantage of microbial therapy over directly ingesting their beneficial compounds is that living bacteria can produce these molecules at the right time and in the right place, ensuring optimal delivery, localization, and effect,” Tropini said. For example, rather than trying to painstakingly determine the dosing regimen for depleted short-chain fatty acids, the gut microbiome could be supplemented with microbial members that have the ideal metabolite production procedures built in. Similarly, adding microbes that activate sex hormones could enable naturally regulated synthesis of testosterone, circumventing the risks surrounding hormone replacement therapy. Manipulation of the gut microbiome also provides a lever by which to target the brain, which is difficult to access with peripheral drugs due to the physical barrier between the body and brain.
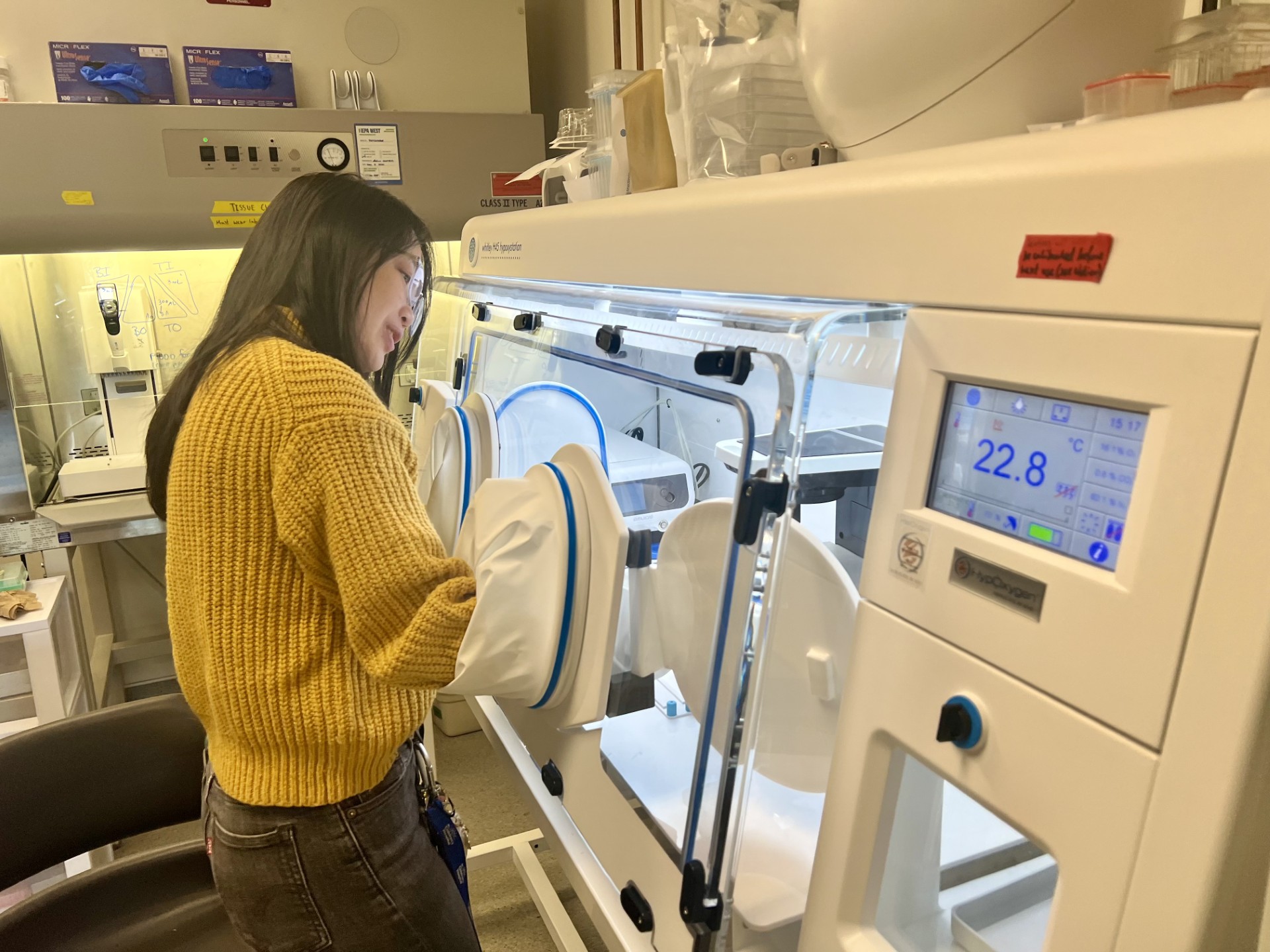
Claire Sie, a PhD student in the Tropini lab and coauthor of the study, works in a hypoxic chamber. "I was really interested in studying how the gut microbiota, this community that's centralized in one place, can signal to these
far-off systems," she said.
Moving forward, the researchers plan to develop strategies to reintroduce specific microbe species to the gut with the goal of attenuating the neurological and endocrine effects of pediatric IBD. But if these microbes are to make a difference, it is critical that they can carve out a niche and thrive within the larger gut microbiome community. “The way that we're approaching microbiota therapies is by thinking about this as a complex ecosystem that we need to support from multiple angles to make it more resilient,” Tropini said. For example, the researchers feed their mice foods rich in fiber, a versatile source of sustenance for a diverse array of microbes, highlighting the importance of similar dietary interventions in humans.
The team is also starting to investigate how the changes in testosterone production they uncovered might influence puberty onset, sperm quality, and fertility later in life. They hope to continue to harness their complimentary areas of expertise to explore new directions in the gut microbiome-neuroendocrine connection. As Ciernia said, “It's only through the synergy between the two groups that you can do this kind of interdisciplinary work, and I think that makes it novel and a lot of fun.”