By Sarah Anderson, PhD
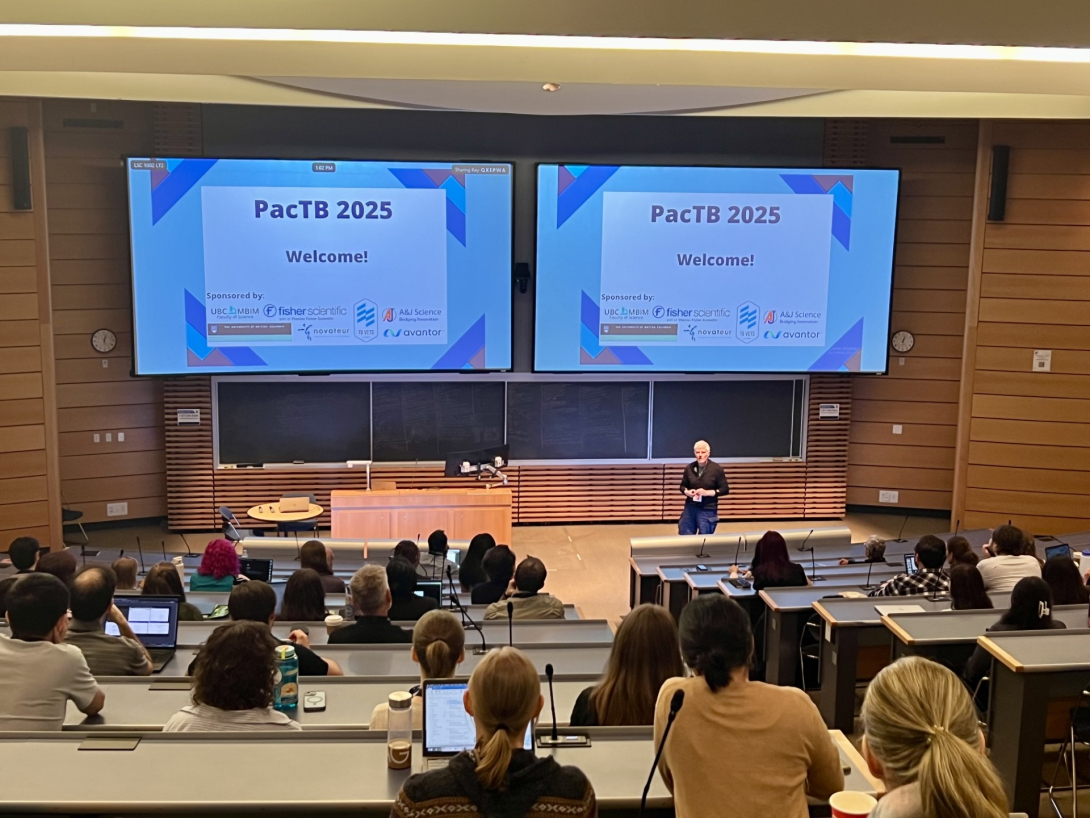
On May 12 and 13, Department of Microbiology and Immunology professors Lindsay Eltis, Jim Sun, and Yossef Av-Gay hosted the 2025 Pacific Tuberculosis Pathogenesis and Host-Response Research Retreat (PacTB). This meeting brings together the west coast community of researchers studying tuberculosis (TB), which is caused by the bacterium Mycobacterium tuberculosis (Mtb), as well as other infections associated with non-tuberculosis mycobacteria. “The goal is to foster collaboration to advance diagnosis, treatment, and prevention of disease. The meeting is also trainee-focused and endeavors to provide them with networking opportunities in a relaxed atmosphere. Thus, a second major objective is empowering and mentoring the next generation of scientists,” Eltis said.
While often perceived as a disease that disappeared in the 1800s, TB remains a very real threat. It is the leading cause of death by an infectious pathogen and latently affects approximately one-fourth of the global population — with more than 80 percent of cases and deaths occurring in low- and middle-income countries. In Canada, TB is especially prevalent within Indigenous Communities, with infection rates among the Inuit People approaching levels seen in places where the disease is endemic. “Drug-resistant strains have contributed to making TB a global health emergency,” Eltis said. “Novel therapies are urgently needed for shorter, efficacious treatment.”
Two researchers from the Department of Microbiology and Immunology gave oral presentations on how they are working toward this aim. Julia Kleetz, a post-doctoral researcher in Eltis’s lab, presented her research investigating how and why Mtb synthesizes a class of lipids known as oxazolones. Mtb produces a diverse array of lipids that form a protective cell envelope which helps the pathogen to persist within and ultimately harm the host. Kleetz is interested in understanding how oxazolone synthesis might contribute to the bacterium’s unique capacity for destruction and how it could serve as a target for new TB therapeutics.

It was not known that bacteria could synthesize oxazolones until 2021, when researchers first identified a cluster of bacterial genes encoding a protein pathway that produces these lipids. This gene cluster belongs to the proteobacteria category of bacteria, which does not include Mtb, but Eltis’s team wondered if groups of genes with a similar evolutionary history might exist in Mtb. They used bioinformatic analysis to identify one such gene cluster in Mtb, and by expressing the cluster in a model organism, observed that the bacterium uses these genes to make oxazolones by modifying the amino acid tyrosine. Kleetz took the same approach to identify an additional gene cluster in Mtb that produces oxazolones from the amino acid tryptophan. “Mtb can produce those oxazolones via two pathways, which emphasizes that they must be of some importance for the bacteria,” Kleetz said.
Kleetz isolated genes encoding individual proteins in these oxazolone synthesis pathways and tested their activity as purified proteins and in different combinations in the model organism. While these experiments illuminated the mechanism by which Mtb produces oxazolones, the function of these lipids remains unclear. Kleetz has evaluated the hypotheses that Mtb produces oxazolones to respond to stress conditions, to facilitate the formation of surface-accumulated microbial communities, or to kill other bacteria that compete for resources, all with negative results. Kleetz next plans to test whether the lipids might be involved in Mtb signalling or scavenging functions.
Leah-Rankine Wilson, a PhD candidate in the Av-Gay lab, presented her research on the dynamic intracellular processes that unfold during the tug-of-war between Mtb and the host’s immune system. Upon infection, macrophage immune cells engulf Mtb, trap it within a membrane bubble known as a phagosome, and acidify the interior of the bubble to kill the bacterium. Mtb launches a unique defense mechanism against this attack, secreting a protein that that blocks the cellular machinery responsible for phagosome acidification. But while biological inhibition of acidification is necessary for Mtb survival, Rankine-Wilson's studies suggest that chemical inhibition could actually kill the bacterium.
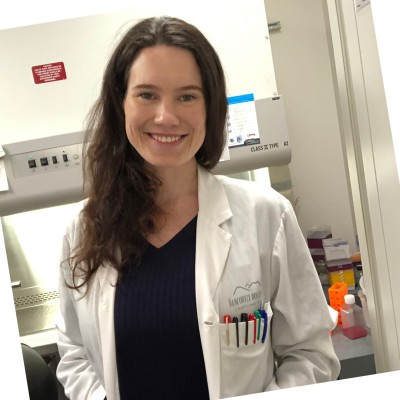
Rankine-Wilson happened upon this unexpected observation while developing a high-content microscopy-based tool to measure phagosome acidification and Mtb growth. She treated infected macrophages with a chemical compound known to inhibit phagosome acidification and discovered that, even while blocking acid-induced death, the compound killed the bacterium. “This finding highlights the complexity of host-pathogen interactions with respect to acidification,” she said.
While this chemical inhibitor has not shown direct antimicrobial activity in the petri dish, Rankine-Wilson is investigating ways in which it may adopt antimicrobial capabilities once inside the host. She has uncovered evidence that the compound may be transformed into an active antibiotic within the immune cell, alter the host response in a way that drives the death of infected cells, and interfere with the bacterial defense mechanisms that are critical for intracellular survival.
Rankine-Wilson's work reveals a new strategy toward improved TB treatment. "I hope my research will contribute to making current antibiotics more effective when administered alongside these acid-reducing compounds,” she said.