In a recent publication in the Journal of Medicinal Chemistry, researchers at the University of British Columbia (UBC) and the Shanghai Institute of Materia Medica (SIMM) joined forces to synthesize a novel compound that shows significant promise in treating tuberculosis (TB).
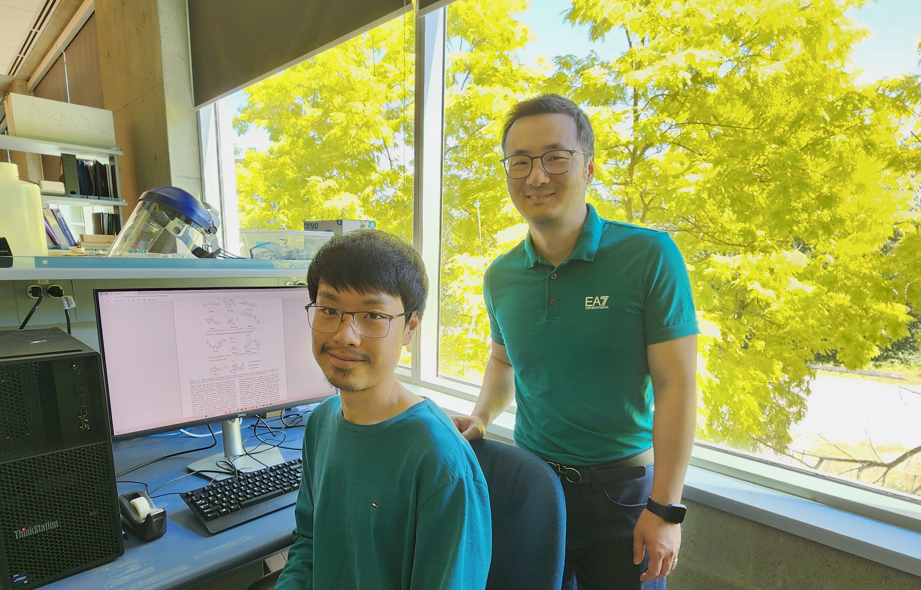
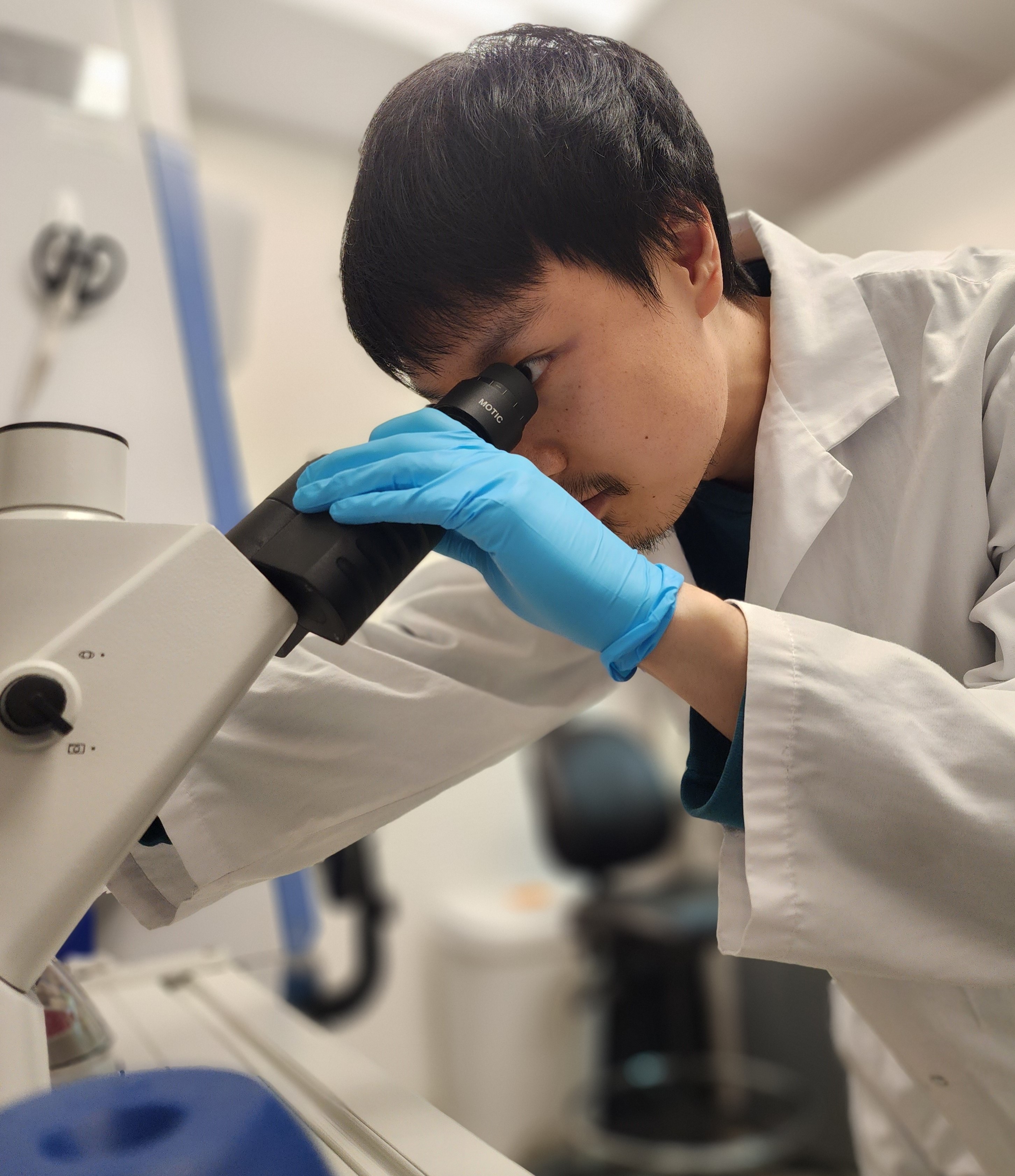
Co-led by PhD student Yichu Liang under the supervision of Dr. Jim Sun (Microbiology & Immunology, UBC), and in collaboration with the medicinal chemistry group of Dr. Weibo Yang (SIMM, Chinese Academy of Sciences), this ground-breaking study suggests that this new compound represents a major advancement for TB drug discovery due to its unique mechanism of action by targeting the host protein PPM1A.
Addressing a Global Health Crisis
Each year, more than 10 million new cases of TB are diagnosed, leading to approximately 1.5 million deaths. The conventional treatments, primarily developed from the 1940s to the early 1960s, necessitate a prolonged regimen of multiple antibiotics spanning several months. To ensure complete eradication of the infection and to avoid the development of drug-resistant TB, patients must adhere to stringent and extended treatment plans.
However, as Dr. Jim Sun states "Mycobacterium tuberculosis, the causative bacteria, is highly capable of manipulating and evading the immune response to hide within our immune cells, where they are shielded from antibiotics." The emergence of drug-resistant Mycobacterium tuberculosis (Mtb) strains demonstrates why TB is so challenging to deal with and has significantly complicated treatment efforts. These new drug-resistant strains require longer treatment durations, often extending up to 18-24 months, with more toxic and expensive medications.
The increased treatment complexity, high cost, and severe side effects of these extended regimens highlight the urgent need for innovative treatment strategies. Novel approaches are essential to combat TB effectively, reduce treatment duration, improve patient compliance, and manage drug-resistant strains. This pressing need drives ongoing research and development efforts to discover and develop new therapeutic agents and strategies.
Thanks to recent collaborative efforts between UBC and SIMM, the research team has developed SMIP-031, a potential breakthrough compound for the treatment of TB.
Host-Directed Therapy
The research team focused on a host-directed therapy (HDT) approach, which aims to bolster the host's immune response rather than directly targeting the pathogen. The benefits of this strategy are that it has the potential to be effective against both drug-susceptible and drug-resistant strains of Mtb and could also help slow the development of further drug resistance.
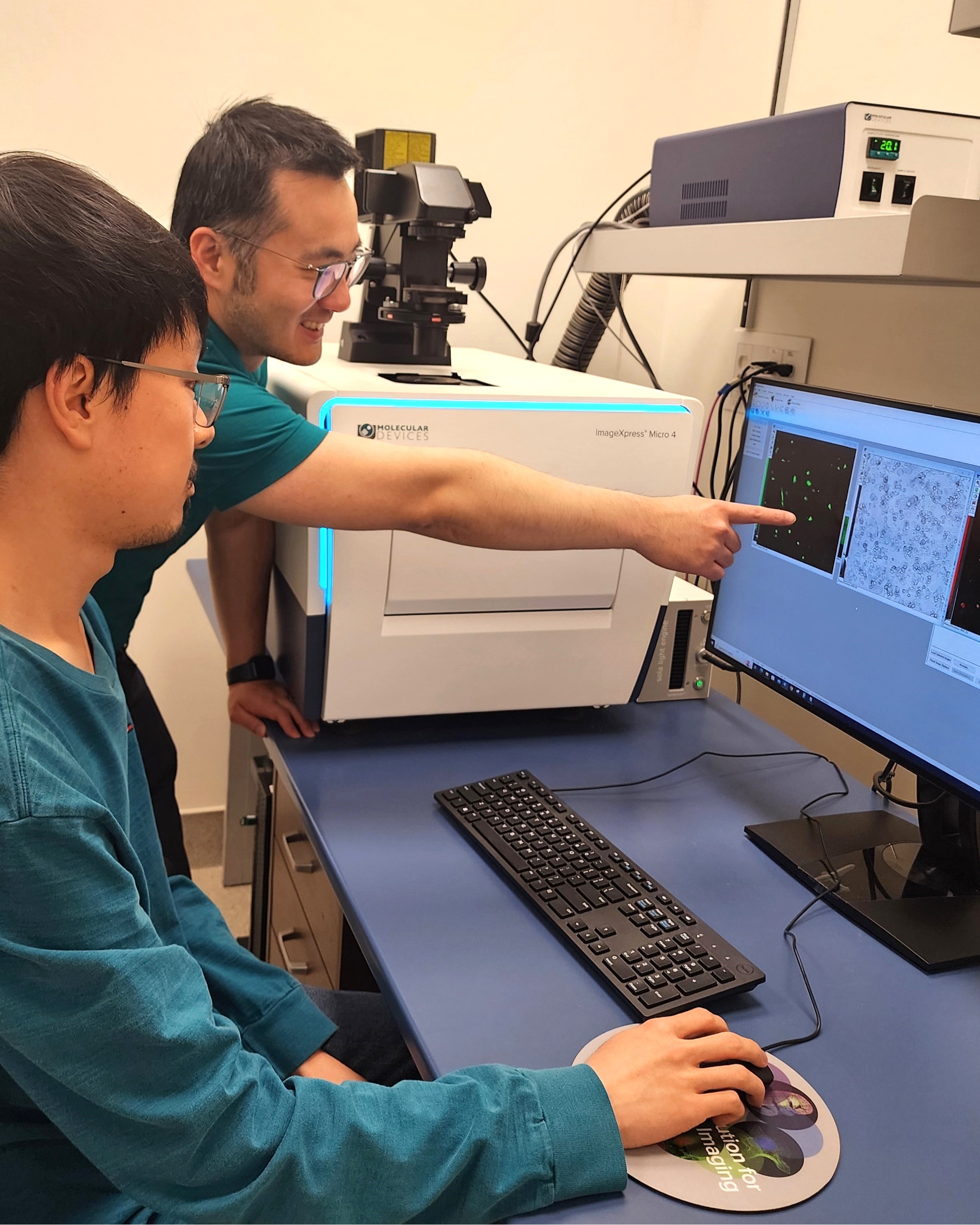
Previously, the team developed SMIP-30, a compound that inhibits the host phosphatase PPM1A, which Mtb uses to survive within macrophages, the host cells it infects. SMIP-30 demonstrated potential by activating autophagy in macrophages, enhancing their ability to kill Mtb, and improving the efficacy of the TB antibiotic rifampicin in mice.
Building on this success, the team redesigned SMIP-30 to create a more potent derivative, SMIP-031. This new compound is ten times more effective as a PPM1A inhibitor and exhibits significantly lower toxicity to host cells. SMIP-031 has demonstrated a four- to five-fold increase in Mtb-killing activity in infected macrophages and is a stronger activator of the autophagy response. Remarkably, SMIP-031 was able to increase Mtb clearance in infected mice on its own, without the need for additional antibiotics.
“That SMIP-031 shows in vivo efficacy on its own is a major step forward for our drug discovery efforts and showcases the power of host-directed therapy for TB.” Yichu Liang remarked.
Potential Impact and Future Directions
The findings from this study indicate that SMIP-031 holds significant promise as a drug candidate for TB treatment. Dr. Jim Sun highlights the potential of these SMIP compounds, stating, "These compounds could essentially make us stronger at fighting off bacterial infections. They could also be combined with existing antibiotics to boost their efficiency and hopefully shorten the duration of treatment, which would have a major impact for TB therapy in the clinics."
Reflecting on the project, Yichu Liang noted, "I began working on this project since joining the Sun Lab at the University of Ottawa five years ago, and brought the project with me to UBC after the lab moved here." He also commented, "It's hard to develop inhibitors against phosphatases, but SMIP-30 (and SMIP-031) showed that not only is PPM1A a viable target, it's also a druggable one."
The research team hopes to develop these SMIP inhibitors further and ultimately create clinically approved treatments that will contribute significantly to the fight against TB and possibly other phosphatase-mediated diseases.
This research was supported by the Canadian Institutes of Health Research, National Sanitarium Association, the University of British Columbia, and the University of Ottawa. Yichu Liang was supported by the CGS-D scholarship from the Natural Sciences and Engineering Research Council of Canada.